Doing battle against Type diabetes
Published February 18, 2010
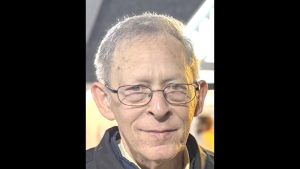
Only about 100 surgeons in this country perform pancreatic transplants, and Dr. Jason Wellen is one of them. Wellen, 35, is director of pancreatic transplantation and an assistant professor of surgery at Washington University School of Medicine/Barnes-Jewish Hospital. He refers to pancreatic transplant surgery as “defying physiology.”
Wellen will speak about his work at 3 p.m. Feb. 20 as part of the Juvenile Diabetes Research Foundation’s annual family retreat. Kathleen Ratchford, one of Wellen’s patients, also will speak. Some 800 people are expected to attend the two-day event, which will be held at the Millennium Hotel, 200 S. 4th Street. (For reservations or more information, call 314-729-1846.)
Formerly known as juvenile diabetes or insulin-dependent diabetes, Type 1 diabetes is a chronic condition in which the pancreas produces little or no insulin. The body needs insulin to allow sugar to enter cells to produce energy. Type 1 diabetes typically appears during adolescence, but can develop at any age. Over time, the disease takes a toll on other organs and systems in the body. There is no cure.
Born in New York, Wellen grew up in South Florida and New York. He attended medical school at St. Georges University School of Medicine in Bayshore, N.Y., did his internship and residency at St. Barnabas Medical Center in Livingston, N.J. and then served as a fellow in abdominal transplant surgery at Washington University School of Medicine/Barnes-Jewish Medical Center. In July, Wellen moved into his current position.
Wellen revealed that his interest in this field developed because he has family members with Type 1 diabetes. He made time recently to explain how pancreatic transplant surgery works – and how it can change people’s lives.
Please explain how this disease works.
Type 1 diabetes is an auto-immune disease. For various reasons, your body attacks cells in the pancreas and stops it from producing insulin. We don’t know why – it could be you’ve been exposed to a virus or it could be an association with several genetic factors – but we do know that 50 million people have Type 1 diabetes.
A pancreatic transplant gives a person with Type 1 diabetes a fresh start. How long has this been going on?
It is sort of a miracle, isn’t it? The surgery was first done in the 1960s, but it wasn’t until the 1980s that doctors started to perfect the surgical technique. Today, between 1,200 and 1,400 pancreatic transplants are done each year across the country.
Does a pancreatic transplant do the trick?
Not by itself. The surgery is almost always for people with Type 1 diabetes who are in renal failure, so 90 percent of pancreatic transplants are done in conjunction with a kidney transplant. Only in select circumstances can I justify transplanting only a pancreas. The most common instance would be when a person’s blood sugar reaches dangerously low levels without any warning, which often results in loss of consciousness or seizures.
How does this combination of surgeries help?
These patients get an improved rate of survival plus several other benefits. The addition of a pancreas has been shown to prolong the kidney transplant’s graft survival and the pancreas will allow the patients to maintain normal blood sugars, significantly improve quality of life and potentially reverse some of the complications of diabetes.
How so?
The surgeries have been shown to reverse some complications of diabetes, including peripheral neuropathy and retinopathy. Also, the transplants can help keep atherosclerosis at bay.
We hear all the time about the shortage of organs needed for transplants. Is there a shortage of pancreases?
There is much less of a shortage than of livers, hearts and kidneys. A person waiting for a kidney may wait three to four years, but if you are on the list for a combined pancreas and kidney transplant, the wait times in this region of the country are less than one year, especially if the pancreas can come from a cadaver donor and the kidney can come from a relative.
What are the risks?
Surgery takes longer — anywhere from five to 10 hours — and the hospitalization is longer, usually seven to 10 days. Also, you’re getting two organs that the body might reject, instead of one. The pancreas is very fickle. It doesn’t like to be played around with, and there is a risk of thrombosis and or bleeding. Sometimes, the pancreas can leak. But there is also a tremendous risk for a diabetic waiting on dialysis.
How do the dual surgeries change people’s lives?
Kidney transplants always change people’s lives tremendously, but a pancreas transplant also gets rid of the diabetes. Afterward, my patients don’t know what to do with themselves – they no longer have to check their blood sugars and they must get accustomed to trying foods with high carbohydrates because suddenly, their function is normal.
How do you get the word out about this exciting treatment option?
As I give talks in the community, I have discovered that even people in the medical field are unaware that we’re doing pancreatic transplants at Washington University-Barnes and how successful our results are. Certainly, programs like the one sponsored by the Juvenile Diabetes Research Foundation are excellent resources for up-to-date information.
Jason R. Wellen, M.D.
WORK: Director of pancreatic transplantation and assistant professor of surgery at Washington University School of Medicine.
HOME: Central West End
FAMILY: Single
HOBBIES: Enjoying Forest Park, biking, running, basketball and cooking
PERSONAL ACCOMPLISHMENT: Helping individuals with Type 1 diabetes to enjoy a better quality of life.