Innovative Israeli breast-cancer treatment uses anesthesia of nervous system around tumor
Published October 23, 2021
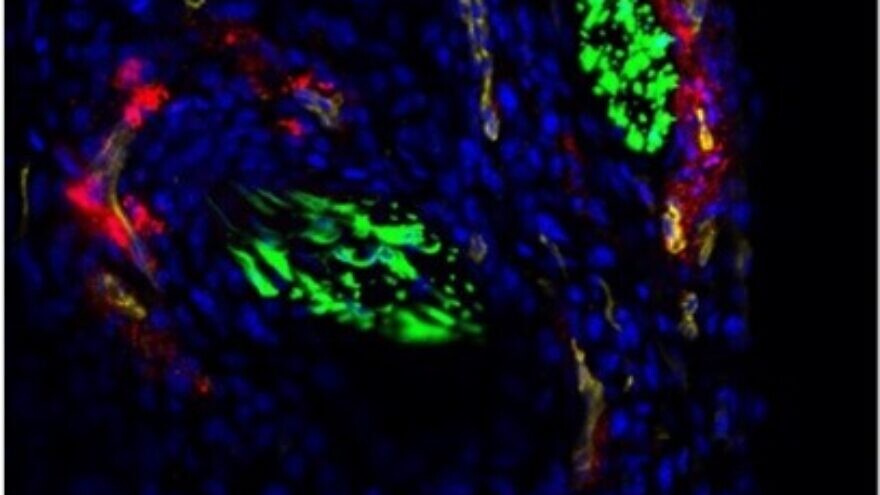
(October 21, 2021 / JNS) Researchers at the Technion‒Israel Institute of Technology have developed an innovative treatment for breast cancer based on analgesic nanoparticles that target the nervous system. The study, published in Science Advances, was led by Professor Avi Schroeder and Ph.D. student Maya Kaduri of the Wolfson Faculty of Chemical Engineering.
Breast cancer is one of the most common cancers in women, and despite breakthroughs in diagnosis and treatment, approximately 1,000 women in Israel die of the disease per year. About 15 percent of them are under the age of 50. Worldwide, it causes some 685,000 deaths annually.
Schroeder has years of experience in developing innovative cancer treatments, including ones for breast cancer—specifically, triple-negative breast cancer, an aggressive type characterized by rapid cell division with a higher risk of metastasis. Technologies developed in his lab include novel methods for encapsulating drug molecules in nanoparticles that transport the drug to the tumor and release it inside without damaging healthy tissue.
ADVERTISEMENT
The researchers found that cancer cells have a reciprocal relationship with the nerve cells around them; the cancer cells stimulate infiltration of nerve cells into the tumor, and this infiltration stimulates cancer-cell proliferation, growth and migration.
In other words, the cancer cells recruit the nerve cells for their purposes.
Based on these findings, the researchers developed a treatment that targets the tumor through the nerve cells based on injecting nanoparticles containing anesthetic into the bloodstream. The nanoparticles travel through the bloodstream towards the tumor, accumulate around the nerve cells in the cancerous tissue, and paralyze the local nerves and communication between the nerve cells and the cancer cells. The result: significant inhibition of tumor development and of metastasis to the lungs, brain and bone marrow.
The nanoparticles simulate the cell membrane and are coated with special polymers that disguise them from the immune system and enable a long circulation time in the bloodstream. Each such particle, which is around 100 nanometers in diameter, contains the anesthetic.
ADVERTISEMENT
“We know how to create the exact size of particles needed, and that is critical because it’s the key to penetrating the tumor,” says Kaduri. “Tumors stimulate increased formation of new blood vessels around them so that they receive oxygen and nutrients, but the structure of these blood vessels is damaged and contains nano-sized holes that enable penetration of nanoparticles. The cancerous tissue is characterized by poor lymphatic drainage, which further increases the accumulation of the particles in the tissue.”
Therefore, she explains, “the anesthetizing particles we developed move through the bloodstream without penetrating healthy tissue. Only when they reach the damaged blood vessels of the tumor do they leak out, accumulate around the nerve cells of the cancerous tissue and disconnect them from the cancer cells. The fact that this is a very focused, precise treatment enables us to insert significant amounts of anesthetic into the body because there is no fear that it will harm healthy and vital areas of the nervous system.”
In experiments on cancer-cell cultures and in the treatment of mice, the new technology inhibited not only tumor development but also metastasis. The researchers estimate that these findings may be relevant for the treatment of breast cancer in humans.